Abstract
Research Article
In vitro antimicrobial activity of a black currant oil based shampoo versus a chlorhexidine 4% shampoo on bacteria strains isolated from canine pyoderma: A comparative study
Antonio Corona*, Paola Persico, Antonella Vercelli, Alessandro Gramenzi and Luisa Cornegliani
Published: 14 April, 2020 | Volume 4 - Issue 1 | Pages: 014-017
Over the last few years, antimicrobial shampoo therapy has been increasingly used to treat skin infections in order to reduce systemic use of antibiotics. This study was aimed to compare the In vitro bactericidal effect of a black currant oil based shampoo (S1) to a chlorhexidine 4% shampoo (S2) against methicillin-sensitive Staphylococcus pseudintermedius (MSSP), methicillin-resistant Staphylococcus pseudintermedius (MRSP), Staphylococcus aureus (SA), Escherichia coli (EC) and Pseudomonas aeruginosa (PA) isolates.
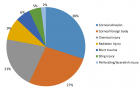
A collection of 50 bacterial strains from skin swabs of dogs with superficial recurrent pyoderma was selected: 10 MSSP, 10 MRSP, 10 SA, 10 EC and 10 PA. The two shampoos were blindly tested in duplicate with a microdilution plate method, with scalar concentrations from 1:2 to 1: 256. The MBC was performed for each dilution. A linear regression was used to detect a statistically significance between the two shampoos.
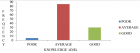
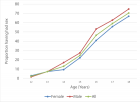
All isolates were completely killed at 1:2 up to 1:16 dilution of the two antiseptic products. At the 1:32 dilution the first bacterial growths were observed, in particular for 2 and 4 strains of MRSP by S1 and S2 respectively. The first lethal dilution for SA was at 1:64 for S1/S2 and only for S2 against SP. No significant difference was observed between the two shampoos according to the results of linear regression significant for: i) MRSP, PA and EC (p < 0.05); ii) MSSP and SA (p < 0.1).
This study showed that both black currant oil based shampoo and chlorhexidine 4% shampoo have a similar In vitro bactericidal activity.
Read Full Article HTML DOI: 10.29328/journal.ivs.1001021 Cite this Article Read Full Article PDF
References
- Rosenkrantz W. Practical applications of topical therapy for allergic, infectious, and seborrheic disorders. Clin Tech Small Anim Pract. 2006; 21: 106–116.PubMed: https://www.ncbi.nlm.nih.gov/pubmed/16933477
- Guaguere E. Topical treatment of canine and feline pyoderma. Vet Dermatol. 1996; 7: 145–51.
- Layne EA. Can pyoderma in dogs be treated with fewer antibiotics? Vet Rec. 2019; 184: 736-738. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/31197051
- Bajwa J. Canine superficial pyoderma and therapeutic considerations. Can Vet J. 2016; 57: 204-206. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4713004/
- Papadogiannakis E, Velonakis E, Vatopoulos A. Ever-increasing emergence of multi-drug resistant Staphylococcus pseudintermedius in the dog and its zoonotic potentials. J Hellenic Vet Medical Soc. 2018; 67: 109-116.
- Miller WH, Griffin CE, Campbell KL. Dermatologic Therapy. In: Muller & Kirk’s Small Animal Dermatology. 7th ed. St. Louis: Elsevier, 2013; 108–183.
- Beco L, Guaguère E, Lorente Méndez C, Noli C, Nuttall T, et al. Suggested guidelines for using systemic antimicrobials in bacterial skin infections: part 2 antimicrobial choice, treatment regimens and compliance. Vet Rec. 2013; 19: 72–78. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/23292948
- Hillier A, Lloyd DH, Weese JS, Blondeau JM, Boothe D, et al. Guidelines for the diagnosis and antimicrobial therapy of canine superficial bacterial folliculitis (Antimicrobial Guidelines Working Group of the International Society for Companion Animal infectious Dis- eases). Vet Dermatol. 2014; 25: 163–175. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24720433
- Hillier A, Alcorn JR, Cole LK, Kowalski JJ. Pyoderma caused by Pseudomonas aeruginosa infection in dogs: 20 cases. Vet Dermatol. 2006; 17: 432–439. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17083575
- Loeffler A, Linek M, Moodley A, Guardabassi L, Sung JM, et al. First report of multiresistant, mecA-positive Staphylococcus intermedius in Europe: 12 cases from a veterinary dermatology referral clinic in Germany. Vet Dermatol. 2007; 18: 412–421. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17991158
- Guardabassi L, Houser GA, Frank LA. Guidelines for antimicrobial use in small animals. In: Guardabassi L, Jensen LB, Hilde K. eds. Guide to Antimicrobial Use in Animals. Oxford: Blackwell Pub. 2008: 183–206.
- Scott DW. Clinical assessment of topical benzoyl peroxide in treatment of canine skin diseases. Vet Med Small Anim Clin. 1979; 74: 808–813. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/256688
- Scott DW, Miller WH, Cayatte SM. A clinical study on the effect of two commercial veterinary benzoyl peroxide shampoos in dogs. Canine Practice 1994; 19: 7–10.
- Bond R, Rose JF, Ellis JW, Lloyd DH. Comparison of two shampoos for treatment of Malassezia pachydermatis associated seborrhoeic dermatitis in basset hounds. J Small Anim Pract. 1995; 36: 99–104. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/7783442
- Lloyd DH, Lamport AI. Activity of chlorhexidine shampoos In vitro against Staphylococcus intermedius, Pseudomonas aeruginosa and Malassezia pachydermatis. Vet Rec 1999; 144: 536–537. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10378283
- Noli C, Carta G, Cordeddu L, Melis MP, Murru E, et al. Conjugated linoleic acid and black currant seed oil in the treatment of canine atopic dermatitis: a preliminary report. Vet J. 2007; 173: 413-421. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/16495095
- Marchegiani A, Fruganti A, Spaterna A, Dalle Vedove E, Bachetti B, et al. Impact of Nutritional Supplementation on Canine Dermatological Disorders. Vet Sci. 2020; 7: E38. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32260299
- Devriese LA, Hermans K, Baele M, Haesebrouck F. Staphylococcus pseudintermedius versus Staphylococcus intermedius. Vet Microbiol. 2009; 133: 206-207. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18760884
- Clinical Laboratory and Standard Institute. Performance standards for antimicrobial disk and dilution susceptibility tests for bacteria isolated from animals: approved standards – 4th edition. CLSI document VET01-A4. Wayne, PA: CLSI; 2013.
- Horstmann C, Mueller RS, Straubinger RK, Werckenthin C. Detection of methicillin-resistant Staphylococcus pseudintermedius with commercially available selective media. Lett Appl Microbiol. 2012; 54: 26-31. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/22023239
- Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012; 18: 268-281. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/21793988
- Guardabassi L, Ghibaudo G, Damborg P. In vitro antimicrobial activity of a commercial ear antiseptic containing chlorhexidine and Tris–EDTA. Vet Dermatol. 2009; 21: 282-286. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/20030799
- Swinney A1, Fazakerley J, McEwan N, Nuttall T. Comparative In vitro antimicrobial efficacy of commercial ear cleaners. Vet Dermatol. 2008; 19: 373–379. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/19055612
- CLSI, Methods for Determining Bactericidal Activity of Antimicrobial Agents. Approved Guideline, CLSI document M26-A. Clinical and Laboratory Standards Institute, 950 West Valley Roadn Suite 2500, Wayne, Pennsylvania 19087, USA, 1998.
- Balouiri M, Sadiki M, Ibnsouda SK. Methods for In vitro evaluating antimicrobial activity: A review. J Pharm Anal. 2016; 6: 71-79. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/29403965
- Swinney A, Fazakerley J, McEwan N et al. Comparative In vitro antimicrobial efficacy of commercial ear cleaners. Vet Dermatol 2008; 19: 373–379. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/19055612
- Lloyd DH, Lamport AI. Activity of chlorhexidine shampoos In vitro against Staphylococcus intermedius, Pseudomonas aeruginosa and Malassezia pachydermatis. Vet Rec. 1999; 144: 536–537. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10378283
- Loeffer A, Lloyd DH. What has changed in canine pyoderma? A narrative review. Vet J. 2018; 235: 73-82. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/29704943
- Oliveira AMP, Devesa JSP, Hill PB. In vitro efficacy of a honey‐based gel against canine clinical isolates of Staphylococcus pseudintermedius and Malassezia pachydermatis. Vet Dermatol. 2018; 29: 180-e65. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/29569291
- Widén C, Renvert S, Persson GR. Antibacterial activity of berry juices, an In vitro study. Acta Odontol Scand. 2015; 73: 539-543. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/25727734
- Miladinović B, Kostić M, Šavikin K, Đorđević B, Mihajilov-Krstev T, et al. Chemical profile and antioxidative and antimicrobial activity of juices and extracts of 4 black currants varieties (Ribes nigrum L). J Food Sci. 2014; 79: 2014. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24506271
- Bourdeau P, Blumstein P, Marchand AM, Gardeyc L, Jasmin P, et al. An in vivo procedure to evaluate antifungals agents on Malassezia pachydermatis in dogs: example with a piroctone olamine containing shampoo. J de Mycologie Médicale. 2006; 16: 9-15.
Figures:
Figure 1
Similar Articles
-
Exploring novel medical applications for commonly used veterinary drug (tilmicosin antibiotic)Fatma I Abo El-Ela*,El-Banna HA. Exploring novel medical applications for commonly used veterinary drug (tilmicosin antibiotic). . 2017 doi: 10.29328/journal.ivs.1001001; 1: 001-016
-
Investigation on Theileria lestoquardi infection among sheep and goats in Nyala, South Darfur State, SudanOsman TM,Ali AM*,Hussein MO,El Ghali A,Salih DA. Investigation on Theileria lestoquardi infection among sheep and goats in Nyala, South Darfur State, Sudan. . 2017 doi: 10.29328/journal.ivs.1001002; 1: 017-023
-
Mechanism-related Teratogenic, Hormone Modulant and other Toxicological effects of Veterinary and agricultural surfactantsAndrás Székács*. Mechanism-related Teratogenic, Hormone Modulant and other Toxicological effects of Veterinary and agricultural surfactants. . 2017 doi: 10.29328/journal.ivs.1001003; 1: 024-031
-
Efficacies of 11% Lactoferricin and 0.05% Chlorhexidine Otological Solution compared, in the treatment of microbial otic overgrowth: A randomized single blinded studyLuisa Cornegliani*,Federico Leone,Francesco Albanese,Mauro Bigliati,Natalia Fanton,Antonella Vercelli. Efficacies of 11% Lactoferricin and 0.05% Chlorhexidine Otological Solution compared, in the treatment of microbial otic overgrowth: A randomized single blinded study. . 2017 doi: 10.29328/journal.ivs.1001004; 1: 032-041
-
Ocular surface Rose Bengal staining in normal dogs and dogs with Keratoconjunctivitis Sicca: Preliminary findingsWilliams DL*,Griffiths A. Ocular surface Rose Bengal staining in normal dogs and dogs with Keratoconjunctivitis Sicca: Preliminary findings. . 2017 doi: 10.29328/journal.ivs.1001005; 1: 042-046
-
Influence of Vitamin E on the Disposition Kinetics of Florfenicol after single and multiple oral administrations in Broiler ChickensFatma Ibrahim Abo El-Ela*,Hossny Awad El-Banna,Manal B El-Deen,Tohamy MA. Influence of Vitamin E on the Disposition Kinetics of Florfenicol after single and multiple oral administrations in Broiler Chickens. . 2017 doi: 10.29328/journal.ivs.1001006; 1: 047-057
-
Effects of carazolol on electrocadiographic and trace element status in sheepsRemzi Gonul,Lora Koenhemsı,Handan Aydın Vural*,Tevfik Gulyasar,Hasret Demırcan Yardıbı,Erman OR,Bora Barutcu. Effects of carazolol on electrocadiographic and trace element status in sheeps. . 2018 doi: 10.29328/journal.ivs.1001007; 2: 001-004
-
Livestock insurance a tool to reduce economical loss of farmers from climate change related HazardsAnanta Koirala*,Priyanka Bhandari. Livestock insurance a tool to reduce economical loss of farmers from climate change related Hazards. . 2018 doi: 10.29328/journal.ivs.1001008; 2: 005-008
-
The failure to provide an effective veterinary service to sheep in AustraliaJAL Maxwell*. The failure to provide an effective veterinary service to sheep in Australia. . 2018 doi: 10.29328/journal.ivs.1001009; 2: 009-017
-
Does Veterinary Science have a future in Australia?JAL Maxwell*. Does Veterinary Science have a future in Australia?. . 2018 doi: 10.29328/journal.ivs.1001010; 2: 018-026
Recently Viewed
-
Transumbilical Single-incision Hiatal Hernia Repair and Nissen Fundoplication in situs Inversus Totalis: A Rare Case ReportQing Cao,Chen Kang,Kang Gu,Yin Peng,Yang Lv,Xu-Zhong Ding,Peng Li*. Transumbilical Single-incision Hiatal Hernia Repair and Nissen Fundoplication in situs Inversus Totalis: A Rare Case Report. Adv Treat ENT Disord. 2026: doi: 10.29328/journal.ated.1001017; 10: 001-003
-
NAD⁺ Biology in Ageing and Chronic Disease: Mechanisms and Evidence across Skin, Fertility, Osteoarthritis, Hearing and Vision Loss, Gut Health, Cardiovascular–Hepatic Metabolism, Neurological Disorders, and MuscleRizwan Uppal,Umar Saeed*,Muhammad Rehan Uppal. NAD⁺ Biology in Ageing and Chronic Disease: Mechanisms and Evidence across Skin, Fertility, Osteoarthritis, Hearing and Vision Loss, Gut Health, Cardiovascular–Hepatic Metabolism, Neurological Disorders, and Muscle. Ann Clin Endocrinol Metabol. 2026: doi: 10.29328/journal.acem.1001032; 10: 001-009
-
Treatment Outcome in Patients with Myofascial Orofacial Pain: A Randomized Clinical TrialAnders Wänman*, Susanna Marklund, Negin Yekkalam. Treatment Outcome in Patients with Myofascial Orofacial Pain: A Randomized Clinical Trial. J Oral Health Craniofac Sci. 2024: doi: 10.29328/journal.johcs.1001046; 9: 001-008
-
Anxiety and depression as an effect of birth order or being an only child: Results of an internet survey in Poland and GermanyJochen Hardt*,Lisa Weyer,Malgorzata Dragan,Wilfried Laubach. Anxiety and depression as an effect of birth order or being an only child: Results of an internet survey in Poland and Germany. Insights Depress Anxiety. 2017: doi: 10.29328/journal.hda.1001003; 1: 015-022
-
Case Report of a Child with Beta Thalassemia Major in a Tribal Region of IndiaNeha Chauhan, Prakash Narayan, Mahesh Narayan, Manisha Shukla*. Case Report of a Child with Beta Thalassemia Major in a Tribal Region of India. J Child Adult Vaccines Immunol. 2023: doi: 10.29328/journal.jcavi.1001011; 7: 005-007
Most Viewed
-
Impact of Latex Sensitization on Asthma and Rhinitis Progression: A Study at Abidjan-Cocody University Hospital - Côte d’Ivoire (Progression of Asthma and Rhinitis related to Latex Sensitization)Dasse Sery Romuald*, KL Siransy, N Koffi, RO Yeboah, EK Nguessan, HA Adou, VP Goran-Kouacou, AU Assi, JY Seri, S Moussa, D Oura, CL Memel, H Koya, E Atoukoula. Impact of Latex Sensitization on Asthma and Rhinitis Progression: A Study at Abidjan-Cocody University Hospital - Côte d’Ivoire (Progression of Asthma and Rhinitis related to Latex Sensitization). Arch Asthma Allergy Immunol. 2024 doi: 10.29328/journal.aaai.1001035; 8: 007-012
-
Causal Link between Human Blood Metabolites and Asthma: An Investigation Using Mendelian RandomizationYong-Qing Zhu, Xiao-Yan Meng, Jing-Hua Yang*. Causal Link between Human Blood Metabolites and Asthma: An Investigation Using Mendelian Randomization. Arch Asthma Allergy Immunol. 2023 doi: 10.29328/journal.aaai.1001032; 7: 012-022
-
An algorithm to safely manage oral food challenge in an office-based setting for children with multiple food allergiesNathalie Cottel,Aïcha Dieme,Véronique Orcel,Yannick Chantran,Mélisande Bourgoin-Heck,Jocelyne Just. An algorithm to safely manage oral food challenge in an office-based setting for children with multiple food allergies. Arch Asthma Allergy Immunol. 2021 doi: 10.29328/journal.aaai.1001027; 5: 030-037
-
Snow white: an allergic girl?Oreste Vittore Brenna*. Snow white: an allergic girl?. Arch Asthma Allergy Immunol. 2022 doi: 10.29328/journal.aaai.1001029; 6: 001-002
-
Cytokine intoxication as a model of cell apoptosis and predict of schizophrenia - like affective disordersElena Viktorovna Drozdova*. Cytokine intoxication as a model of cell apoptosis and predict of schizophrenia - like affective disorders. Arch Asthma Allergy Immunol. 2021 doi: 10.29328/journal.aaai.1001028; 5: 038-040

If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."